How is a blood test normally done?
- The vein used for blood sampling is usually on the inside of your elbow or the back of your wrist.
- A tight band (tourniquet) is usually placed around your upper arm. This makes the vein fill with blood and makes it easier for the blood sample to be taken.
- The skin over the vein may be cleaned with an antiseptic wipe.
- A needle is then inserted into the vein through the clean skin causing a sharp pricking sensation. The needle is connected either to a syringe, or directly to blood sample bottles.
- When the required amount of blood is taken, the needle is removed. The small wound is pressed on with cotton wool for a few minutes to stop the bleeding and prevent bruising. A sticking plaster may be put on. The blood is placed in bottles. There may be a slight ache following a blood test.
Variations of blood taking
- Some blood tests require several samples taken over a period of time. For example, they may be done to check how you respond to something. If you require repeated samples fairly close to each other (over the following few hours or so), a doctor may insert a 'butterfly' needle into the vein, which can be taped to the skin. Samples of blood can then be taken without using a needle each time.
- If only a small amount of blood is needed then a few drops of blood can be squeezed out from a small prick in the tip of the finger or earlobe. For example, only a small amount of blood is needed for checking the blood sugar (glucose) level, using a test strip of paper.
- Some blood tests are taken from an artery in the wrist. For example, to measure the level of oxygen in the artery. This is usually only done in hospital in certain circumstances
- You may be told not to eat for a time before certain tests. For example, a test of blood glucose is commonly done first thing in the morning before you have anything to eat.
- Children who need a blood test may be given cream to put on at home before the test to numb the skin.
Are there any complications from blood taking?
- Sometimes a bruise develops where the needle was inserted. This is much less likely to happen if you press over the site with cotton wool for several minutes with your arm left straight (not bent).
- As with any wound, an infection may develop where the needle was inserted. See your doctor if the wound site becomes red and inflamed.
- Rarely, some people feel faint during a blood test. Tell the person doing the test if you feel faint, as you should immediately lie down to prevent fainting.
Different blood samples
Blood can be tested for many different things. The person who requests the blood test will write on the form which tests they want the laboratory to do. Different blood bottles are used for different tests. For example, for some tests the blood needs to clot and the test is looking for something in the serum. For some tests, the blood is added to some chemicals to prevent it from clotting. If the blood glucose is being measured, then the blood is added to a special preservative, etc. This is why you may see your blood added to blood bottles of different sizes and colours.
Blood tests are taken for many different reasons - for example, to:
- Help diagnose certain conditions, or to rule them out if symptoms suggest possible conditions.
- Monitor the activity and severity of certain conditions. For example, a blood test may help to see if a condition is responding to treatment.
- Check the body's functions such as liver function and kidney function when you are taking certain medicines which may affect the liver or the kidneys.
- Check your blood group before receiving a blood transfusion
What is a full blood count (FBC)?
An FBC is one of the most common blood tests done. A blood sample is taken which is prevented from clotting by using a preservative in the blood bottle. The sample is put into a machine which automatically:
- Counts the number of red cells, white cells and platelets per millilitre of blood.
- Measures the size of the red blood cells and calculates their average (mean) size.
- Calculates the proportion of blood made up from red blood cells (the haematocrit).
- Measures the amount of haemoglobin in the red blood cells.
The main abnormalities which can be detected are:
- Anaemia - this means that you have fewer red blood cells than normal, or have less haemoglobin than normal in each red blood cell. The most common reason for an FBC to be done is to check for anaemia. There are many causes of anaemia. The average size of the red cells can give a clue as to the cause of some anaemias.. (Iron is needed to make haemoglobin.) With this type of anaemia, the average size of the red blood cells is smaller than normal.
- Too many red cells - this is called polycythaemia and can be due to various causes.
- Too few white cells - this is called leukopenia. Depending on which type of white cell is reduced it can be called neutropenia, lymphopenia or eosinopenia. There are various causes.
- Too many white blood cells - this is called leukocytosis. Depending on which type of
white cell
is increased it is called neutrophilia, lymphocytosis, eosinophilia, monocytosis or basophilia.
There are various causes - for example:
- Various infections can cause an increase of white blood cells.
- Certain allergies can cause an eosinophilia.
- Leukaemia is a type of blood cancer where there is a large number of abnormal cells, usually white blood cells. The type of leukaemia depends on the type of white cell affected.
- Too few platelets - this is called thrombocytopenia. This may make you bruise or bleed easily. There are various causes.
- Too many platelets - this is called thrombocythaemia (or thrombocytosis). This is due to disorders which affect cells in the bone marrow which make platelets.
The Kidneys
The kidneys regulate the amount of water and salts that we have in our bodies. They do this by filtering the blood through millions of structures called nephrons. The kidneys also pass out certain waste products from the body. Urine is made up of the excess water, salts and waste products passed out by the kidneys down to the bladder.
The usual blood test which checks that the kidneys are working properly measures the level of urea, creatinine and certain dissolved salts.
Urea is a waste product formed from the breakdown of proteins. Urea is usually passed out in the urine. A high blood level of urea ('uraemia') indicates that the kidneys may not be working properly, or that you have a low body water content (are dehydrated).
Creatinine is a waste product made by the muscles. Creatinine passes into the bloodstream, and is usually passed out in urine. A high blood level of creatinine indicates that the kidneys may not be working properly. Creatinine is usually a more accurate marker of kidney function than urea. The effect of muscle mass needs to be taken into account. A person with a lot of muscle and little fat on their body is likely to have a higher creatinine than a person who has a lot of fat and little muscle.
Estimated glomerular filtration rate (eGFR) provides a guide to kidney function. Although the level of creatinine in the blood is a useful guide to kidney function, the eGFR is a more accurate measure. Blood creatinine can be used to estimate the eGFR using age, sex and race. This is often calculated by computer and reported with the creatinine blood test. The normal value for eGFR is 90-120 ml/min. An eGFR below 60 ml/min suggests that some kidney damage has occurred. The value becomes lower with increasing severity of kidney damage
Liver Function Tests
Liver function tests measure various chemicals in the blood made by the liver. An abnormal result may indicate a problem with your liver and may help to identify the cause. Further tests may be needed to clarify the cause of your liver problem.
What does the liver do?
The liver is in the upper right part of your tummy (abdomen). The functions of your liver include:
- Storing fuel for your body (called glycogen) which is made from sugars.
- Helping to process fats and proteins from digested food.
- Making proteins that are essential for your blood to clot (clotting factors).
- Processing many medicines which you may take.
- Helping to remove poisons and toxins from your body.
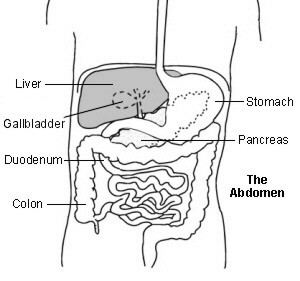
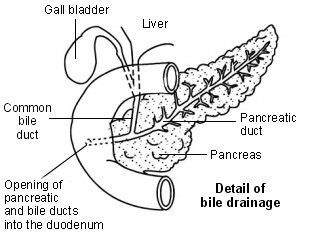
The liver also makes bile. This is a greenish-yellow fluid that contains bile acids, bile pigments and waste products such as bilirubin. Liver cells pass bile into bile ducts inside the liver. The bile flows down these ducts into larger and larger ducts, eventually leading to the common bile duct. The gallbladder is like a 'cul-de-sac' reservoir of bile which comes off the common bile duct. After you eat, the gallbladder squeezes bile back into the common bile duct and down into the the first part of the gut, known as the duodenum. Bile in the gut helps to digest fats.
What are liver function tests (LFTs)?
As the liver performs its various functions, it makes chemicals that pass into the bloodstream. Various liver disorders alter the blood level of these chemicals. Some of these chemicals can be measured in a blood sample.
LFTs are some tests that are commonly done on a blood sample. These usually measure the following:
- Alanine transaminase (ALT). This is an enzyme that helps to process proteins. (An enzyme is a protein that helps to speed up chemical reactions. Various enzymes occur in the cells in your body.) Large amounts of ALT occur in liver cells. When your liver is injured or inflamed (as in hepatitis), the blood level of ALT usually rises.
- Aspartate aminotransferase (AST). This is another enzyme usually found inside liver cells. When a blood test detects high levels of this enzyme in your blood it usually means your liver is injured in some way. However, AST can also be released if heart or skeletal muscle is damaged. For this reason, ALT is usually considered to be more specifically related to liver problems.
- Alkaline phosphatase (ALP). This enzyme occurs mainly in liver cells next to bile ducts, and in bone. The blood level is raised in some types of liver and bone disease.
- Albumin. This is the main protein made by your liver and it circulates in your bloodstream. The ability to make albumin (and other proteins) is affected in some types of liver disorder. A low level of blood albumin occurs in some liver disorders. It can also occur in people who are malnourished.
- Total protein. This measures albumin and all other proteins in blood.
- Bilirubin. This chemical gives bile its yellow/green colour. A high level of bilirubin in
your blood will make you appear 'yellow' (jaundiced). Bilirubin is made from haemoglobin.
Haemoglobin is a chemical in red blood cells that is released when your red blood cells break
down. Liver cells take in bilirubin and attach sugar molecules to it. This is then called
'conjugated' bilirubin which is passed into your bile ducts:
- A raised blood level of 'conjugated' bilirubin occurs in various liver and bile duct conditions. It is particularly high if the flow of bile is blocked. For example, by a gallstone stuck in the common bile duct, or by a tumour in the pancreas. It can also be raised with hepatitis, liver injury, or long-term alcohol abuse.
- A raised level of 'unconjugated' bilirubin occurs when there is excessive breakdown of red blood cells - for example, in haemolytic anaemia. It can also occur in people with Gilbert's syndrome which is a common, harmless condition.
The normal range of LFTs can often vary between different laboratories, so it is not always possible to compare results directly if they have been taken at different places. Also, the normal ranges of values for LFTs are often different for men and women.
What are liver function tests (LFTs) used for?
LFTs are used:
- To help diagnose liver disorders if you have symptoms which may be due to liver disease - such as appearing 'yellow' (jaundiced). The pattern of the blood results may help to determine which disorder is causing the problem. For example, depending on which enzyme is highest, it may point to a particular disorder.
- To monitor the activity and severity of liver disorders.
- As a routine precaution after starting certain medicines, to check that they are not causing liver damage as a side-effect.
- To screen for any potential liver disease (for example, in those who are alcohol-dependent or in people who have been exposed to a hepatitis virus).
Tests for Blood Sugar (Glucose) and HbA1c
Measuring blood sugar (glucose) is used to diagnose diabetes. It is also used to monitor glucose control for those people who are already known to have diabetes. If your glucose level remains high then you have diabetes. If the level goes too low then it is called hypoglycaemia.
Urine test for blood sugar (glucose)
Urine (produced by the kidneys) does not normally contain glucose. The kidneys filter our blood, keeping substances the body needs, while getting rid of waste products. Your kidneys constantly reabsorb glucose so that it doesn't enter your urine. However, if the glucose level goes above a certain level, the kidneys can't reabsorb all of the glucose. This means that some glucose will 'spill' through the kidneys into the urine.
A simple dipstick test can detect glucose in a sample of urine. In a dipstick test a doctor or nurse uses a special chemical strip which he/she dips into a sample of your urine. Colour changes on the strip show whether there is glucose in the urine sample. If you have glucose in your urine, you are likely to have diabetes.
However, some people have kidneys that are more 'leaky' and glucose may leak into urine with a normal blood level. Therefore, if your urine contains any glucose, you should have a blood test to measure the blood level of glucose to confirm, or rule out, diabetes.
Blood tests for blood sugar (glucose)
Random blood glucose level
A sample of blood taken at any time can be a useful test if diabetes is suspected. A level of 11.1 mmol/L or more in the blood sample indicates that you have diabetes. A fasting blood glucose test may be done to confirm the diagnosis.
Fasting blood glucose level
A glucose level below 11.1 mmol/L on a random blood sample does not rule out diabetes. A blood test taken in the morning before you eat anything is a more accurate test. Do not eat or drink anything except water for 8-10 hours before a fasting blood glucose test. A level of 7.0 mmol/L or more indicates that you have diabetes.
If you have no symptoms of diabetes but the blood test shows a glucose level of 7.0 mmol/L or more, the blood test must be repeated to confirm you have diabetes. If you do have symptoms and the blood test shows a glucose level of 7.0 mmol/L or more, the test does not need to be repeated. See the separate leaflets called Type 1 Diabetes and Type 2 Diabetes for more details.
The HbA1c blood test
If you have diabetes, your HbA1c level may be done every 2-6 months by your doctor or nurse. This test measures your recent average blood sugar (glucose) level. The test measures a part of the red blood cells. Glucose in the blood attaches to part of the red blood cells. This part can be measured and gives a good indication of your average blood glucose over the previous 2-3 months.
For people with diabetes, treatment aims to lower the HbA1c level to below a target level which is usually agreed between you and your doctor. Ideally, the aim is to maintain your HbA1c to less than 48 mmol/mol (6.5%). However, this may not always be possible to achieve and the target level of HbA1c should be agreed on an individual basis between you and your doctor. (For example, by increasing the dose of medication, improving your diet, etc.)
It is now recommended that HbA1c can also be used as a test to diagnose diabetes. An HbA1c value of 48 mmol/mol (6.5%) or above is recommended as the blood level for diagnosing diabetes. People with an HbA1c level of 42-47 mmol/mol (6.0-6.5%) are at increased risk of diabetes and cardiovascular disease.
Blood Tests to Detect Inflammation
Inflammation and blood proteins
If you have inflammation in a part of your body then extra protein is often released from the site of inflammation and circulates in the bloodstream. The erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and plasma viscosity (PV) blood tests are commonly used to detect this increase in protein. In this way they are used as markers of inflammation.
Erythrocyte sedimentation rate, C-reactive protein and plasma viscosity blood tests
Erythrocyte sedimentation rate (ESR)
A blood sample is taken and put in a tube that contains a chemical to stop the blood from clotting. The tube is left to stand upright. The red blood cells (erythrocytes) gradually fall to the bottom of the tube (as a sediment). The clear liquid plasma is left at the top. The ESR measures the rate at which the red blood cells separate from the plasma and fall to the bottom of a test tube. The rate is measured in millimetres per hour (mm/hr). This is easy to measure as there will be a number of millimetres of clear liquid at the top of the red blood after one hour.
If certain proteins cover red cells, these will stick to each other and cause the red cells to fall more quickly. So, a high ESR indicates that you have some inflammation, somewhere in the body.
Levels of ESR are generally higher in females. Also the level increases with increasing age.
C-reactive protein (CRP)
This is sometimes called an acute phase protein. This means that the level of CRP increases when you have certain diseases which cause inflammation. CRP can be measured in a blood sample. The CRP test measures the level of one specific protein, whereas the ESR takes account of many proteins.
Plasma viscosity (PV)
The conditions which the ESR test monitors can also be monitored by the PV test. It is another marker of inflammation. However, it is more difficult to perform and is not as widely used as ESR testing.
What conditions affect the erythrocyte sedimentation rate and C-reactive protein level?
Raised ESR, CRP and PV levels are all markers of inflammation. Generally, PV and ESR do not change as rapidly as CRP does, either at the start of inflammation or as it goes away. CRP is not affected by as many other factors as the PV or ESR, making it a better marker of some types of inflammation. PV, however, is more sensitive and more specific than either ESR or CRP when monitoring the activity of rheumatoid arthritis.
ESR, CRP and PV can be raised in many inflammatory conditions - for example:
- Certain infections (mainly bacterial infections).
- Abscesses.
- Rheumatoid arthritis.
- Various other muscular and connective tissue disorders - for example, polymyalgia rheumatica, giant cell arteritis or systemic lupus erythematosus.
- Tissue injury and burns.
- Some cancers- for example myeloma and Hodgkin's lymphoma.
- Crohn's disease.
- Rejection of an organ transplant.
- After operations.
Some conditions lower the ESR - for example, heart failure, polycythaemia, and sickle-cell anaemia. It is also lowered in conditions where your body has lower protein levels - for example, in some liver or kidney diseases.
When are these tests used?
To help diagnose diseases
ESR, CRP and PV are nonspecific tests. In other words, a raised level means that 'something is going on' but further tests will be needed to clarify exactly what that is. For example, you may be unwell but the cause may not be clear. A raised ESR, CRP and PV may indicate that some inflammatory condition is likely to be the cause. This may prompt a doctor to do further tests to find the cause.
It is not usually possible to make a diagnosis of a certain condition just from a raised ESR, CRP or PV level.
However, before you have further tests, your doctor may suggest that you have the ESR, CRP or PV test repeated after a period of several weeks or months. If it has been raised by a recent infection (a very common cause) then it is likely to return to normal when your infection improves. You would not then need any further tests.
To monitor the activity of certain diseases
For example, if you have polymyalgia rheumatica, the amount of inflammation and disease activity can partially be assessed by measuring one of these blood tests. As a rule, the higher the level, the more active the disease. The response to treatment may also be monitored, as the level of ESR, CRP and PV may fall if the condition is responding well to treatment.
All three tests are useful. However, changes in the CRP are more rapid. So, for example, a fall in the CRP within days of starting treatment for certain conditions is a useful way of knowing that treatment is working. This may be important to know when treating a serious infection or a severe flare-up of an inflammatory condition. For example, if the CRP level does not fall, it may indicate that the treatment is not working and may prompt a doctor to switch to a different treatment.
Cholesterol
What is cholesterol?
Cholesterol is a fat chemical (lipid) that is made in the cells in your body. Many different cells make cholesterol but cells in the liver make about a quarter of the total. You need some cholesterol to keep healthy.
Although many foods contain cholesterol, it is poorly absorbed by the gut into the body. Therefore, cholesterol that you eat in food has little effect on your body and blood cholesterol level.
A certain amount of cholesterol is present in the bloodstream. Cholesterol is carried in the blood as part of particles called lipoproteins. There are different types of lipoproteins but the most relevant to cholesterol are:
- Low-density lipoproteins carrying cholesterol (LDL cholesterol). This is often referred to as 'bad' cholesterol. This is the one mainly involved in forming blockages in the arteries (atheroma). Atheroma is the main underlying cause of various cardiovascular diseases (see below). The majority of cholesterol in the blood is LDL cholesterol but how much varies from person to person.
- High-density lipoproteins carrying cholesterol (HDL cholesterol). This is often referred to as 'good' cholesterol. This may prevent atheroma forming.
What factors affect the blood level of cholesterol?
To an extent your blood cholesterol level can vary depending on your diet. However, different people who eat the same diet can have different blood cholesterol levels. In general, however, if you eat less fatty food in your diet your cholesterol level is likely to go down.
In some people a high cholesterol level is due to another condition. For example, an underactive thyroid gland, obesity, drinking a lot of alcohol and some rare kidney and liver disorders can raise the cholesterol level.
In some people a very high level of cholesterol runs in the family, due to a genetic problem with the way cholesterol is made by the cells in your body. One example is called familial hypercholesterolaemia.
Risk factors
Everybody has some risk of developing small fatty lumps (atheroma) within the inside lining of blood vessels, which then may cause one or more cardiovascular diseases. However, some situations increase the risk. These include:
- Lifestyle risk factors that can be prevented or changed:
- Smoking.
- Lack of physical activity (a sedentary lifestyle).
- Obesity.
- An unhealthy diet - including eating too much salt.
- Excess alcohol.
- Treatable or partly treatable risk factors:
- High blood pressure (hypertension).
- High cholesterol blood level. However, only LDL cholesterol is a risk factor. HDL cholesterol is healthy for your body.
- High triglyceride (another type of fat) blood level.
- Diabetes.
- Kidney diseases that affect kidney function.
- Fixed risk factors - ones that you cannot alter
- A strong family history. This means if you have a father or brother who developed heart disease or a stroke before they were 55, or in a mother or sister before they were 65.
- Being male.
- An early menopause in women.
- Age. You are more likely to develop atheroma as you get older.
- Ethnic group. For example, people who live in the UK whose family came from India, Pakistan, Bangladesh or Sri Lanka have an increased risk.
However, if you have a fixed risk factor, you may want to make extra effort to tackle any lifestyle risk factors that can be changed
Note: risk factors interact. So, if you have two or more risk factors, your health risk is much more increased than if you just have one. For example, a middle-aged male smoker who has high blood pressure and a high cholesterol level has a high risk of developing a cardiovascular disease, such as a heart attack, before the age of 60.
Blood Grouping
The main reasons to know your blood group are if you need to have a blood transfusion or if you are pregnant.
What is normal blood made up of?
Blood cells
These can be seen under a microscope and make up about 40% of the blood's volume. Blood cells are divided into three main types:
- Red cells (erythrocytes). These make blood a red colour. One drop of blood contains about five million red cells. A constant new supply of red blood cells is needed to replace old cells that break down. Millions of red blood cells are made each day. Red cells contain a chemical called haemoglobin. This binds to oxygen and takes oxygen from the lungs to all parts of the body.
- White cells (leukocytes). There are different types of white cells which are called neutrophils (polymorphs), lymphocytes, eosinophils, monocytes and basophils. They are part of the immune system. Their main role is to defend the body against infection. Neutrophils engulf germs (bacteria) and destroy them with special chemicals. Eosinophils and monocytes also work by swallowing up foreign particles in the body. Basophils help to intensify inflammation. Inflammation makes blood vessels leaky. This helps specialised white blood cells get to where they are needed. Lymphocytes have a variety of different functions. They attack viruses and other germs (pathogens). They also make antibodies which help to destroy pathogens.
- Platelets. These are tiny and help the blood to clot if we cut ourselves.
Plasma
This is the liquid part of blood and makes up about 60% of the blood's volume. Plasma is mainly made from water but also contains many proteins and chemicals. Antibodies are one of the types of protein found in plasma.
What is a blood group?
Red blood cells (erythrocytes) have certain proteins on their surface, called antigens. Also, your plasma contains antibodies which will attack certain antigens if they are present. ABO and rhesus are both types of antigens found on the surface of red blood cells. There are lots of other types but these are the most important.
ABO types
These were the first type discovered.
- • If you have type A antigens on the surface of your red blood cells, you also have anti-B antibodies in your plasma.
- If you have type B antigens on the surface of your red blood cells, you also have anti-A antibodies in your plasma.
- If you have type A and type B antigens on the surface of your red blood cells, you do not have antibodies to A or B antigens in your plasma.
- If you have neither type A nor type B antigens on the surface of your red blood cells, you have anti-A and anti-B antibodies in your plasma.
It is not known what the functions of the A and B antigens are. People who don't have either (blood group O) are still just as healthy. There is some evidence that people of different blood groups may be more or less susceptible to certain diseases - for example, blood clots in the blood vessels (thromboembolism) and malaria. There is no evidence that people with different blood groups should follow different diets.
Rhesus types
Most people are 'rhesus positive'. This means they have rhesus antigens on their red blood cells. But, about 3 in 20 people do not have rhesus antibodies and are said to be 'rhesus negative'.
Blood group names
Your blood group depends on which antigens occur on the surface of your red blood cells. Your genetic make-up, which you inherit from your parents, determines which antigens are present on your red blood cells. Your blood group is said to be:
- A+ (A positive) if you have A and rhesus antigens.
- A− (A negative) if you have A antigens but don't have rhesus antigens.
- B+ (B positive) if you have B and rhesus antigens.
- B− (B negative) if you have B antigens but don't have rhesus antigens.
- AB+ (AB positive) if you have A, B and rhesus antigens.
- AB− (AB negative) if you have A and B antigens but don't have rhesus antigens.
- O+ (O positive) if you have neither A nor B antigens but you have rhesus antigens.
- O− (O negative) if you don't have A, B or rhesus antigens.
Other blood types
There are many other types of antigen which may occur on the surface of red blood cells. However, most are classed as 'minor' and are not as important as ABO and rhesus.
How is blood group testing done?
Basically, a sample of your blood is mixed with different samples of plasma known to contain different antibodies. For example, if plasma which contains anti-A antibodies makes the red cells in your blood (erythrocytes) clump together, you have A antigens on your blood cells. Or, if plasma which contains rhesus antibodies makes the red cells in your blood clump together, you have rhesus antigens on your blood cells. By doing a series of such tests it is possible to determine what antigens are on your red blood cells and therefore determine your blood group.
Routine blood grouping checks for your ABO and rhesus status. Other red cell antigens are tested for in certain other situations.
Blood transfusions and cross-matching
If you have a blood transfusion, it is vital that the blood you receive is well matched (compatible) with your own. For example, if you receive blood from a person who is A positive and you are B positive, then the anti-A antibodies in your plasma will attack the red blood cells (erythrocytes) of the donated blood. This causes the red cells of the donated blood to clump together. This can cause a serious or even fatal reaction in your body.
Therefore, before a blood transfusion is done, a donor bag of blood is selected with the same ABO and rhesus blood group as yourself. Then, to make sure there is no incompatibility, a small sample of your blood is mixed with a small sample of the donor blood. After a short time the mixed blood is looked at under a microscope to see if there has been any clumping of blood. If there is no clumping, then it is safe to transfuse the blood.
Blood groups and pregnancy
A blood group test is always done on pregnant women. If the mother is rhesus negative and the unborn baby is rhesus positive (inherited from a rhesus positive father) then the mother's immune system may produce anti-rhesus antibodies. These may attack and destroy the baby's blood cells. This is rarely a problem in a first pregnancy. However, without treatment, this can become a serious problem in subsequent pregnancies, as the mother's immune system will be 'sensitised' after the first pregnancy.
Thyroid Function Tests
What is a thyroid function test?
Thyroid function tests are blood tests that check the levels of the chemicals (hormones) made by your thyroid gland. Some thyroid function tests also check the level of a hormone made by the pituitary gland in your brain, which acts on your thyroid gland.
What is the thyroid?
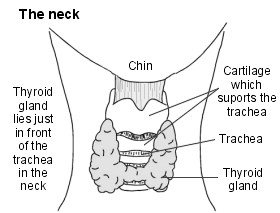
The thyroid is a gland found in your neck. Its main function is to make hormones.
Hormones are chemicals which are released into your bloodstream. They act as messengers, affecting cells and tissues in distant parts of your body. Thyroid hormones affect your body's metabolic rate and the levels of certain minerals in your blood.
What does the thyroid do?
The thyroid makes three hormones which it releases (secretes) into the bloodstream. Two of these hormones, called thyroxine (T4) and triiodothyronine (T3), increase your body's metabolic rate. The other hormone helps to control the amount of calcium in the blood.
In order to make T4 and T3, your thyroid gland needs iodine, a substance found in the food we eat. T4 is called this because it contains four atoms of iodine. T3 contains three atoms of iodine. In the cells and tissues of your body most T4 is converted to T3. T3 is the more active hormone; it influences the activity of all the cells and tissues of your body.
How does the thyroid work?
The main job of your thyroid gland is to produce hormones T4 and T3. To do this your thyroid gland has to take a form of iodine from your bloodstream into your thyroid gland itself. This substance then undergoes a number of different chemical reactions which result in the production of T3 and T4.
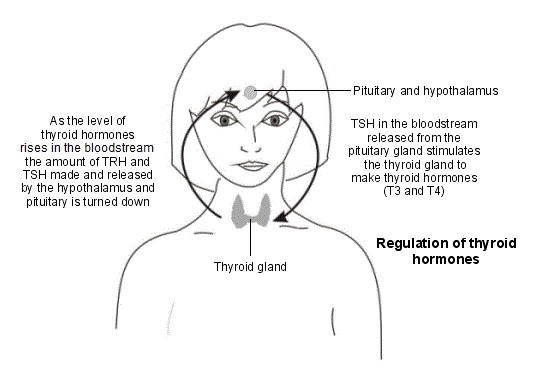
The activity of your thyroid is controlled by chemicals (hormones) produced by two parts of your brain: the hypothalamus and the pituitary. Your hypothalamus receives input from your body about the state of many different bodily functions. When your hypothalamus senses levels of T3 and T4 are low, or that your body's metabolic rate is low, it releases a hormone called thyrotropin-releasing hormone (TRH). TRH travels to your pituitary via your connecting blood vessels. TRH stimulates your pituitary to secrete thyroid-stimulating hormone (TSH).
TSH is released from your pituitary into your bloodstream and travels to your thyroid gland. Here TSH causes cells within your thyroid to make more T3 and T4. T3 and T4 are then released into your bloodstream where they increase metabolic activity in your body's cells.
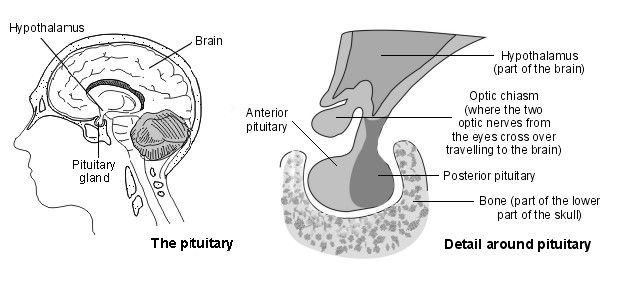
High levels of T3 stop your hypothalamus and pituitary from releasing (secreting) more of their hormones. In turn this stops your thyroid producing T3 and T4. This system ensures that T3 and T4 should only be made when their levels are too low.
How do thyroid function tests work?
There are several different types of thyroid function tests which may be carried out. Interpreting all the different tests is complicated as there are various conditions which can change the level of these chemicals (hormones). A rough guide to the different types of tests and their interpretation is given below. However, your doctor or specialist doctor should explain individual test results.
Usually the first test to check thyroid function measures the levels of TSH in your blood. In people with an under active thyroid (hypothyroidism) the amount of TSH will usually be high. This is usually because the thyroid is not making enough T3 to stop the pituitary producing TSH. If the level of TSH is high, you will usually have further tests to check the levels of T3 and T4 in the blood.
In people with an overactive thyroid (hyperthyroidism) the level of TSH will usually be low. This is usually because the thyroid gland is making too much of its hormones. When levels of T3 and T4 are high, the pituitary is 'turned off' and the amount of TSH produced is less. If you are found to have low levels of TSH you may have some more blood tests to check the levels of T3 and T4 in the blood. These tests may help doctors to find a specific cause of the low TSH.
What are thyroid function tests used for?
Thyroid function tests are usually done to find out whether the thyroid gland is working properly. This is mainly to diagnose an under active thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism).
People with some conditions have an increased risk of thyroid problems and so are often advised to have thyroid function tests undertaken each year. This conditions include:
- Type 1 diabetes
- Coeliac disease
- Addison's disease
- Down's syndrome
- Turner syndrome
Certain drugs can also affect the function of your thyroid - for example, amiodarone and lithium.
Thyroid function tests can also be done to:
- Monitor treatment with thyroid replacement medicine for people who have hypothyroidism.
- Check thyroid gland function in people who are being treated for hyperthyroidism.
- Screen newborn babies for inherited problems with the thyroid.
- What happens during a thyroid function test?
A thyroid function test is a simple blood test. The blood sample is then sent to the laboratory for analysis and the results are sent back to the doctor who asked for the tests.
